“Enhanced recovery” started with the initial work of Henrik Kehlet, a Danish colorectal surgeon, who in the early 2000’s began to challenge many of the traditional surgical practices that were not supported by high-level evidence.
The Enhanced Recovery After Surgery Society (www.erassociety.org), an international, multidisciplinary, not-for-profit organization comprising surgeons, anesthesiologists, nurses and allied health professionals, delivers the ERAS program, and has made recommendations and developed guidelines for colorectal surgeries, gynecologic surgeries, pancreaticoduodenectomy, hepatectomy, gastrectomy, urologic surgery and esophagectomy, all of which have been implemented with good results.
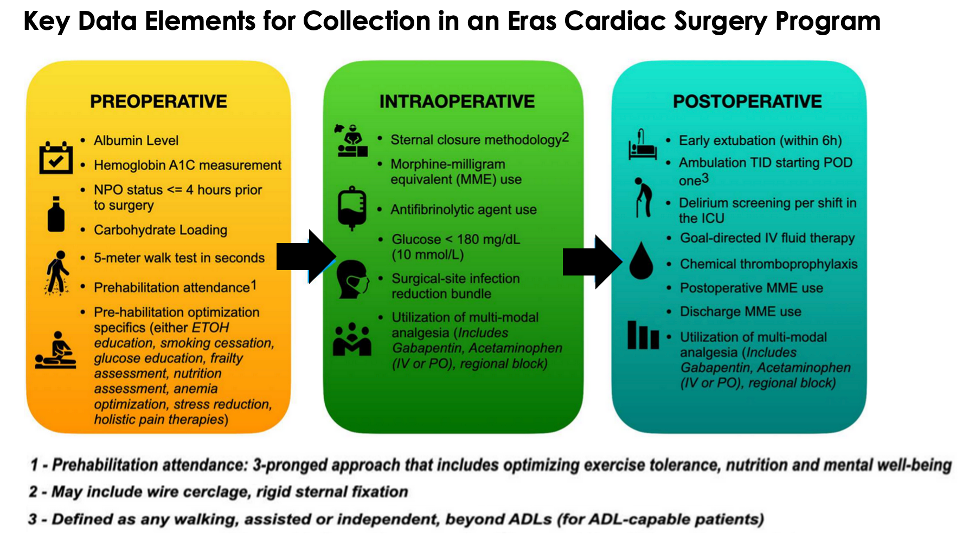
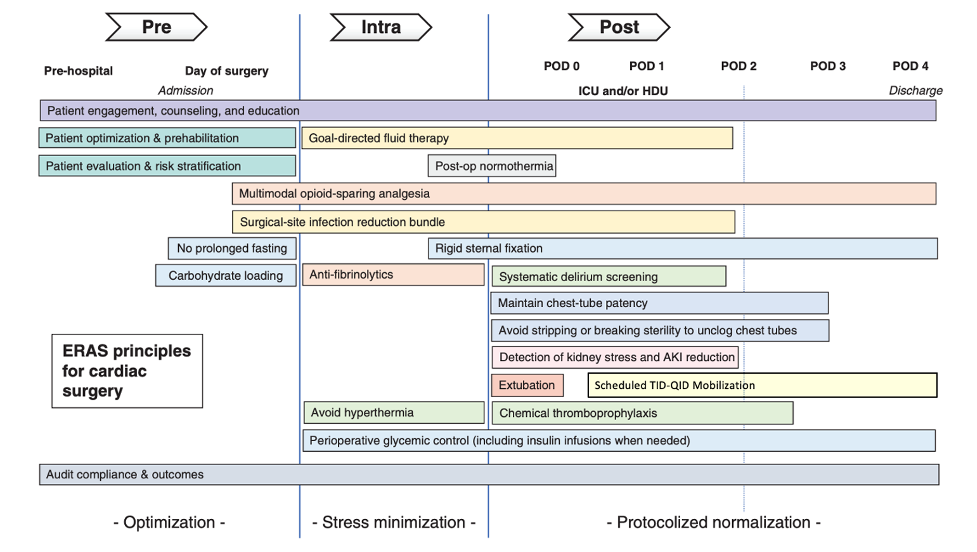
The ERAS approach can be broken down into 3 main components: preoperative, intraoperative, and postoperative. However, enhanced recovery begins with optimizing a patient’s physical status before surgery. Therefore, primary care physicians can support successful implementation of enhanced recovery and help to improve patient outcomes by offering preoperative education and counselling. It is also important to remember that ERAS is a multifaceted approach that should be used for all surgical patients; in other words, anyone receiving a surgical intervention should have an enhanced recovery.
![]()

Enhanced Recovery Canada is a project of the Canadian Patient Safety Institute leading the drive to improve surgical safety across the country and is based on Enhanced Recovery After Surgery – ERAS surgical best practices. These evidence-based principles support better outcomes for surgical patients including: an improved patient experience, reduced length of stay, decreased complication rates and fewer hospital readmissions.
Core ERAS principles to shift the surgical care paradigm:
- Patient and family engagement
- Nutrition management
- Perioperative fluid and hydration management
- Multi-modal opioid sparing analgesia
- Perioperative best practices
- Mobilization

ERAS stands for Enhanced Recovery After Surgery, and we improve surgical care and recovery through research, education, audit, and implementation of evidence-based practices.
In early 2017, a group of cardiac surgeons, anesthesiologists, and intensivists first met to establish the Enhanced Recovery After Cardiac Surgery (ERACS) Society to achieve these goals for patients undergoing heart surgery. This initial organization’s work led to the publication of the first-ever expert consensus recommendations for a cardiac surgical enhanced recovery protocol. We have since joined with the ERAS Society and have established an organization of multinational experts representing all aspects of healthcare delivery.
ERAS Cardiac is a non-profit organization with the mission to develop evidence-based expert consensus statements promoting best practice recovery practices. The goal is to provide hospitals with better guidance for developing local protocols that are part of a continuous quality improvement process for better patient care and reduce postoperative complications and costs after heart surgery.

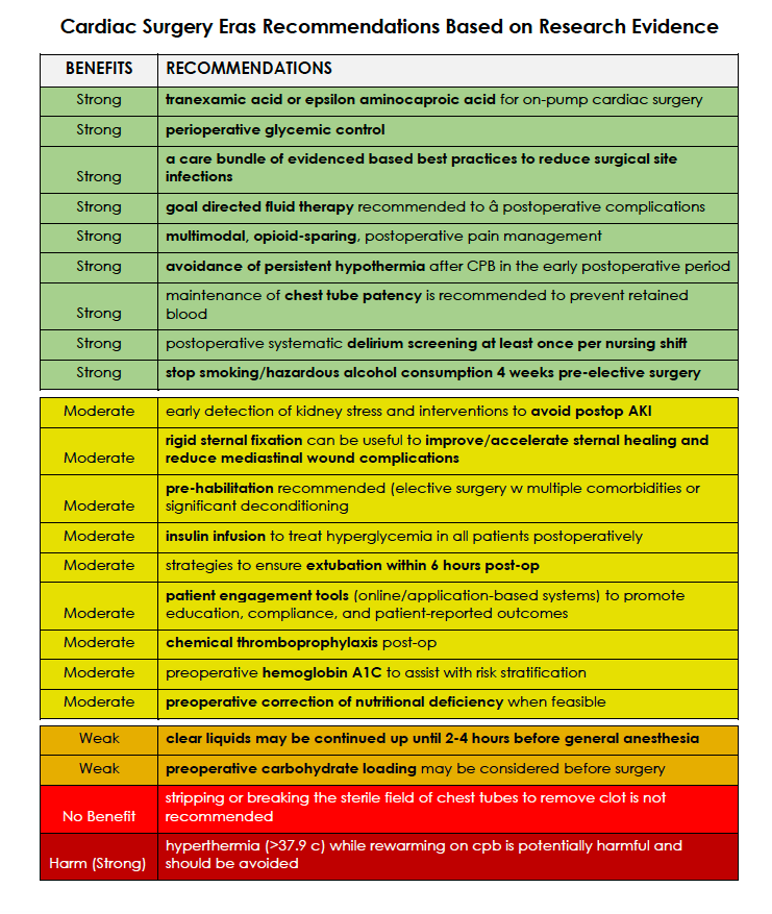
Preoperative phase - Optimization
• Patient engagement, counseling and education
• Preoperative optimization of comorbidities and prehabilitation
• Decreased use or cessation of alcohol and tobacco products
• Preoperative optimization of nutritional status
• No prolonged fasting; Preoperative fasting for 8 hours except for Carbohydrate loading
(CHO) loading 2 to 4 hours before surgery
• Preoperative initiation of multimodal analgesic
• Minimization of anxiolytic agents
• Audit compliance and outcomes
Intraoperative phase - Intraoperative Stress Minimization
• Patient engagement, counseling and education
• Goal directed fluid therapy, Minimization of intraoperative crystalloid
• Post-op normothermia
• Multimodal opioid-sparing analgesia
• Intraoperative opioid administration
• Intraoperative multimodal analgesia
• Initiation of postoperative sedation
• Surgical site infection reeducation bundle
• Anti-fibrinolytics
• Rigid sternal fixation
• Perioperative glycemic control – including insulin infusions when needed
Postoperative phase - Protocolized Normalization (POD 0, 1(ICU), 2, 3, 4 D/C)
• Patient engagement, counseling and education
• Goal directed fluid therapy
• Early extubation
• Scheduled TID or QID mobilization
• Optimization of pulmonary function
• Continuation of Multimodal opioid- sparing analgesia
• Early mobilization to chair and ambulating as tolerated
• Post-op normothermia
• Rigid sternal fixation
• Prophylaxis to prevent postoperative nausea and vomiting
• Maintain chest-tube patency – avoid stripping or breaking sterility to unclog chest tubes
• Detection of kidney stress and AKI reduction
• Chemical thromboprophylaxis
• Perioperative glycemic control – including insulin infusions when needed
• Diet advanced as tolerated
• Bowel motility regimen
• Removal of lines and drains as soon as no longer needed
• Systemic delirium screening
• Surgical site infection reeducation bundle
Primary Outcomes - Reduction post-op complications from:
• prolonged ventilation
• hospital acquired infections
• re-operations
• stroke
• renal failure
• atrial fibrillation ileus
• death
Secondary Outcomes - Reduced
• hospital readmissions (all cause)
• ICU length of stay
• hospital length of stay
• costs associated with hospital stay
• post-op opioid use; improved pain management & pain scores