Ticks and Mites
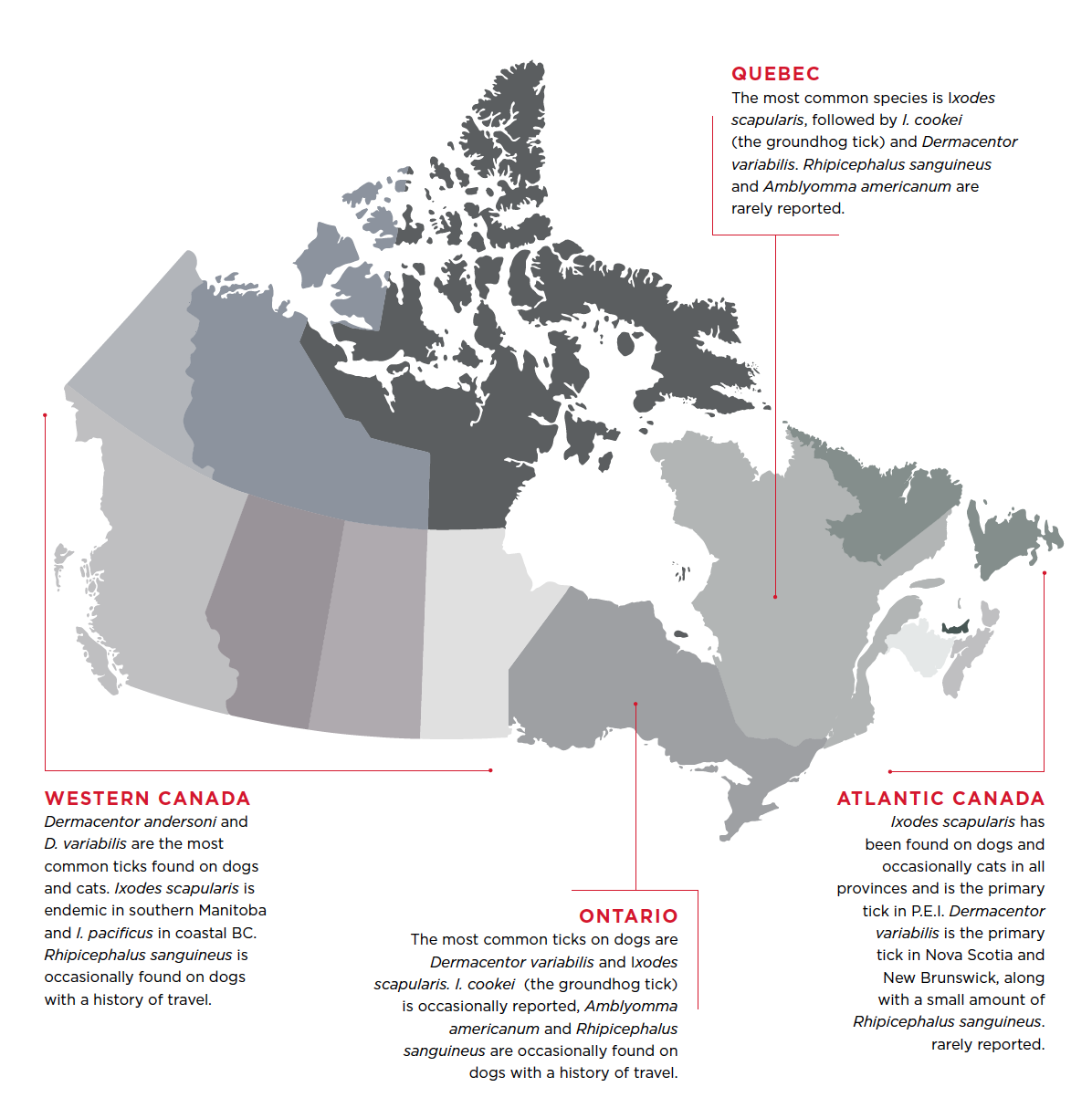
The distribution and abundance of tick species varies widely in Canada, and the geographic range of some species is expanding.
In many regions, an increasing number of ticks have been observed on people and pets. This is likely due to a combination of an actual increase in tick abundance along with greater awareness of tick-borne illnesses and therefore greater surveillance effort. Dogs and cats at greatest risk are pets with access to suitable tick habitat (brush, long grass) in areas with high abundance of suitable wildlife maintenance hosts.
In areas of Canada endemic for Ixodes scapularis, >15% of I. scapularis (sometimes > 50%) are typically infected with Borrelia burgdorferi, the causative agent of Lyme disease (Bouchard et al 2015). Ixodes scapularis may transmit other pathogens, such as Anaplasma. Outside endemic areas, cases of Lyme disease and anaplasmosis in dogs are rare and are thought to be due to either travel or seasonal introduction of I. scapularis by migratory birds. Because it takes years to confirm the establishment of an endemic population of ticks, Public Health Ontario has adopted risk area mapping to provide up-to-date information on the distribution of I. scapularis and the associated public health hazards. An estimated risk area is defined as a 20-km radius around a locality where adult ticks have been found in two consecutive tick seasons.
Tick species in Canada (below)
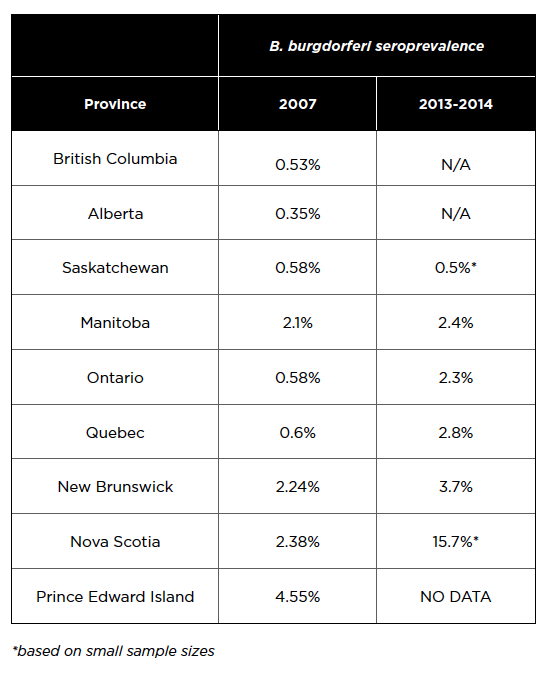
The prevalence of tick-borne disease in Canada’s dog population remains quite low and dogs are generally at very low risk of becoming infected and of developing clinical disease. B. burgdorferi seroprevalence in a population of 115,636 Canadian dogs tested from 2013-2014 (Herrin et al 2017) is compared below to data from 94,928 samples tested in 2007 (as determined by the IDEXX SNAP® 3Dx® and 4Dx® Tests – 2007 National Incidence Study Results, IDEXX, Markham, ON). The following data do not distinguish travel acquired cases and indicate only the province of testing.
Seroprevalence for B. burgdorferi appears to be on the rise for some provinces, although these results are difficult to interpret due to lack of statistical significance, travel history, denominators for testing, and denominators for total dog and cat populations in the province. As well, these data indicate exposure and not necessarily current infection. Many dogs that seroconvert for B. burgdorferi do not develop clinical signs. In addition, the true prevalence of exposure within Canada is likely to be lower than the reported estimates for several reasons: there is no evidence that confirmatory tests were done for any of the samples; the travel history of dogs is not given; and, in light of the very low prevalence of infection in most areas, some positive results may be false positives. A useful reference on this topic is the ACVIM consensus update on Lyme borreliosis in dogs and cats (Littman et al 2018).
At the time of publication, there is no evidence of established populations of Ixodes scapularis in BC, AB, SK, and the northern territories. At the time of publication, there is also no evidence to suggest that there are established populations of Amblyomma americanum in Canada. This tick is encountered sporadically in eastern Canada and may be associated with a travel history, or a tick that has fallen off a migratory bird. However, vigilance is recommended along the US border in eastern Canada. All veterinarians should be comfortable identifying the main genera of ticks commonly encountered on pets in their area, to assess risk of tick-borne illness and to detect introductions of exotic tick species.
The tick season varies depending on regional climate and tick species of concern. Dermacentor spp. adults are most commonly active in the late spring and summer, when they are found on pets and people. In regions where I. scapularis nymphs are introduced via migratory birds, adult I. scapularis are generally found on pets and people in the fall. In endemic regions, I. scapularis are most active in spring and fall (adults) and early summer months (nymphs). I. scapularis (adults) can be active any time the ambient temperature rises above 4°C. Between 2010 and March 2018, in Ontario, only the month of February 2015 failed to see ambient temperatures reach 4°C, and in Quebec, only January and February 2015 failed to reach this threshold. In Nova Scotia, all months since 2010 have seen at least 1 day >4°C. Therefore, it is recommended that a tick preventive be administered even during winter months if temperatures rise above this threshold level in regions endemic for I. scapularis.
Many products with rapid action against ticks are available for preventing infestation. Tick control products should be prescribed based on a regional, seasonal, and individual risk assessment that includes knowledge of tick species
and tick-borne illnesses endemic in the region. There are numerous tick treatment and preventative products that may be used. Tick species vary widely across Canada, and not all products are effective against all tick species so carefully read the label when selecting a product to fit your patient’s needs. Products containing pyrethroids are generally not safe for use in cats and should not be used on dogs in households with cats (see exception in flea section above). Note that tick preventives do not always provide 100% protection for the entire inter-treatment period and may need to be applied more frequently to maintain efficacy in areas where ticks are plentiful. Pet owners should also be advised that they may see a low number of ticks on an animal even after treatment, particularly near the end of the efficacy period.
Prevention
In tick-endemic regions, veterinarians should remind pet owners of the following measures to avoid ticks and tick-borne diseases, in the following order, according to risk of the pet and risk perception of the owner.
- The first line of defense is avoidance; litter under forest canopies, overgrown grass and brush in yards, especially during periods of high tick activity (seasonally and diurnally).
- Second is regular checking and removal of ticks from pets and people within 6-24 hours of being in tick-infested areas.
- Wearing protective clothing such as long pants, long sleeves and socks will help prevent tick attachment to people.
- To remove an attached tick, use tweezers to grasp its “head” and mouth parts as close to the skin as possible. Pull slowly until the tick is removed. Do not twist or rotate the tick and try not to damage or crush the body of the tick during removal. After removing the tick, wash the site of attachment with soap and water and/or disinfect it with alcohol or household antiseptic. (Reference: www.canada.ca/en/public-health/services/diseases/lyme-disease.html)
- Third, there are a wide range of tick control products for high risk dogs and repellents for people. Permethrin treated clothing may also be an option for high risk people.
- Finally, high risk dogs can also be vaccinated against B. burgdorferi, consistent with recommendations of the ACVIM.
- Treatment and management of B. burgdorferi positive dogs should be conducted in accordance with the ACVIM Consensus Update on Lyme borreliosis in Dogs and Cats (2018) in conjunction with the original ACVIM Consensus Statement on Lyme Disease in Dogs: Diagnosis, Treatment, and Prevention (2006).
