Airway submucosal gland dysfunction is a primary defect in CF that may contribute to airway pathobiology. Airway submucosal glands contribute most of the mucus and antimicrobial factors in the upper airways, which are important for the normal lung host defense function. There is increasing evidence that submucosal glands function abnormally in the CF airways. Thus, it has been proposed that CF airways suffer from reduced delivery of antimicrobial factors and mucus that would abate mucociliary clearance and facilitate infection.
However, the response of airway submucosal glands to inhalation of bacteria has never been directly tested. One of the main obstacles to study bacteria-airway interaction in situ is the lack of suitable techniques with appropriate resolution and contrast. There is substantial evidence that synchrotron-based phase contrast imaging (PCI) and diffraction enhanced imaging (DEI) can be used to investigate the air/fluid interface in the lung. The large differences in refractive index between the air and fluids/tissue give a very strong refraction signature that is easily detected using phase related imaging methods.
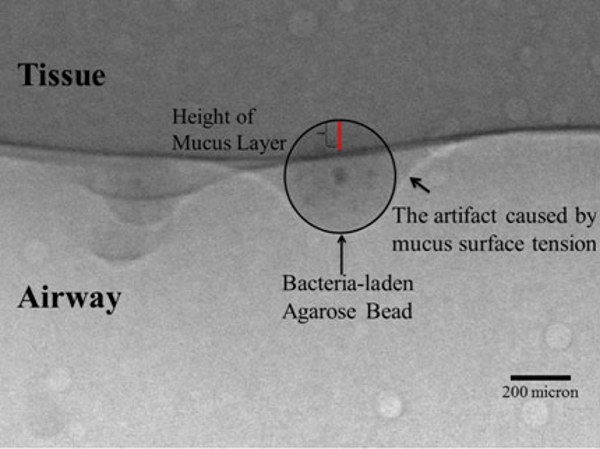
Our objective is to use synchrotron-based phase related imaging methods to image the air/mucus interface in isolated tracheas to study the effects of bacteria-laden agarose beads on submucosal glands mucus secretion. Our results show that synchrotron-related PCI and DEI technique can be used to image the air and mucus interfaces in isolated tracheas. Although it is hard to visualize the mucus/tissue interface, we manage to determine the position of the tissue relative to the mucus layer using agarose beads loaded with the contrast agent barium sulfate.

