assiniskwew: Woman of the Rock
Indigenous Achievement Week 2021
Originally recorded February 2, 2021
Monica Goulet shares her journey with kidney disease in this webinar recorded as part of Indigenous Achievement Week at the University of Saskatchewan. This event was co-hosted by the Indigenous Admission Program in the College of Medicine, the College of Nursing, and the Saskatchewan Indigenous Mentorship Network.
COVID-19
COVID-19 Vaccination in Transplant Recipients
Originally recorded January 15, 2021
Melanie Dieudé, PhD, Executive Director, Canadian Donation and Transplantation Research Program presents to the First Nations and Metis Organ Donation and Transplantation Network
Open House
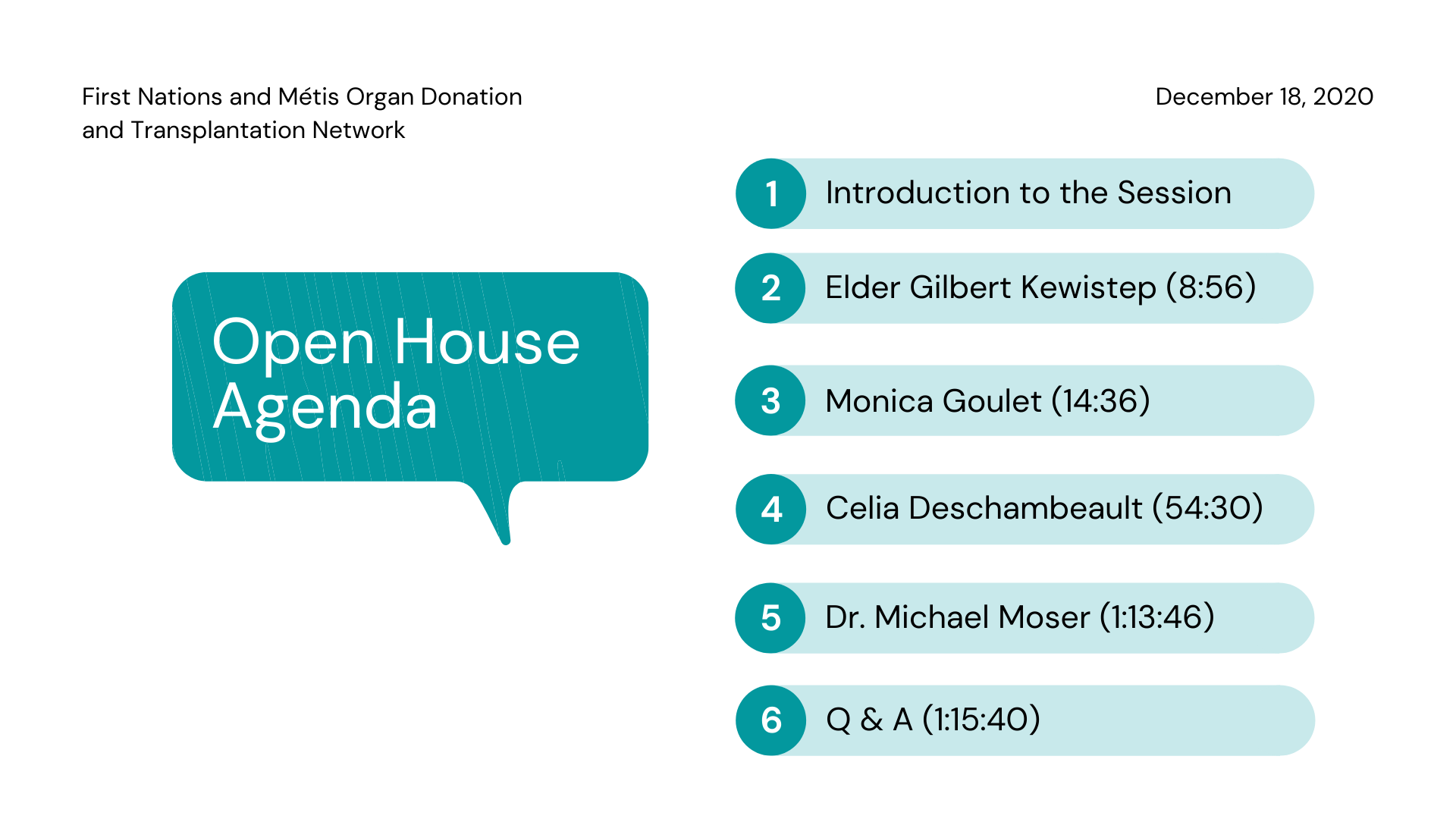
December 18, 2020
We hosted our first Online Open House on December 18, 2020. See below for the participant's stories and the full open house video. Thank you to Elder Gilbert Kewistep for opening our meeting in a good way and to our speakers, Monica Goulet, Celia Deschambeault and Dr. Mike Moser and to all who participated!
Monica
Celia
Full Open House
Think Tank Members
We are a robust and growing team of Elders, Community members, persons with lived experience, researchers, physicians, and students who are all committed to furthering a conversation of Indigenous perspectives on organ donation and transplantation. We feel this topic is particularly salient given the higher representation of Indigenous peoples on transplant wait lists in Saskatchewan, and the announcement of a provincial organ donation registry.
| Celia Deschambault | Lived experience | Swampy Cree |
| Mary Jane Kasyon | Lived experience | Dene |
| Sandra Youngchief | Lived experience | Métis |
| Monica Goulet | Lived experience | Métis |
| Nettie Littlechief-King | Lived experience | Cree |
| Ernest Sauvé | Elder/Thought Leader | Cree |
| Gilbert Kewistep | Elder/Thought Leader | Saulteaux |
| Judy Pelly | Elder/Thought Leader | Cree |
| Eugene Arcand | Elder/Thought Leader | Cree/FN |
| Vivian Meabry | Elder/Thought Leader | Métis |
| Terri Hansen-Gardiner | Elder/Thought Leader | Métis |
| Evelyn Johnston | Elder/Thought Leader | Métis |
| Patti Tait | Elder/Thought Leader | Anishinaabe |
| Dr. Michael Moser | Transplant Surgeon, Researcher | Settler |
| Dr. Caroline Tait | Medical Anthropologist, Researcher | Métis |
| Dr. Joanne Kappel |
Nephrologist (kidney doctor), Co-lead CAN-Solve
|
Settler |
| Carmen Levandoski | Outreach Worker | Settler |
| Dr. Adam McInnes | Physician, Bioengineering PhD student | Métis |
| Jacqueline Smith | Network Graduate Research Assistant | Swampy Cree |
CBS Grant - Liver Leading Practice
Liver Transplant and Alcohol Use Study
Until recently, people with alcohol-related liver disease who needed a liver transplant had to stop using alcohol and other substances for six months before their names could be added to a wait list for a transplant. Doctors and healthcare managers thought that people with alcohol-related liver disease needed to make lifestyle changes before being offered the opportunity to have life-saving surgery. Medical professionals thought that abstinence (stopping drinking) would improve a person’s chances of surviving a transplant, or that the liver, when no longer exposed to alcohol, would repair itself so that the person no longer needed a transplant. Now we are finding that these assumptions are not only incorrect, but also discriminatory.
Compared to the general public, First Nations and Métis people in Canada are more likely to be diagnosed with liver disease and have higher rates of alcohol use, but are less likely to receive a liver transplant. We want to ensure that First Nations and Métis peoples’ perspectives are included in decisions that will affect how and when people living with alcohol use disorder will be considered eligible for transplants.
Canadian Blood Services has initiated a nation-wide study to identify what kinds of guidelines around alcohol use would be acceptable to clinicians, healthcare professionals, and patients. As part of this national study, our research focuses on the thoughts and experiences of First Nations and Métis Elders, knowledge keepers, potential patients and their families. We want to ensure that the thoughts and experiences of Indigenous people are included in new guidelines, as these guidelines will affect their eligibility for transplants.
There are different ways to participate, depending on what kind of experience you have had with liver disease and alcohol use:
- People living with alcohol use disorder, or who have alcohol-related liver disease and need a transplant can participate in focus groups or interviews. We are offering an honorarium for your participation. Close family members are also able to participate in this research; contact us for more information.
- Healthcare service providers who work with First Nations and Metis patients that have alcohol-related liver disease and require a transplant can participate in interviews.
If you would like to find out more, or want to arrange an interview or register for a focus group, fill out the form linked here, or email josediego.marquessantos@usask.ca.
RUH Foundation Grant
Organ Donation and Transplantation: Examining Culturally Safe Public Health Education and Health Care Services with Indigenous Peoples

SHRF/SCPOR Sprout Grant
Donation and Transplantation: Examining Culturally Safe Public Health Education and Health Care Services with Indigenous Peoples
Due to high rates of disease, Saskatchewan First Nations and Metis people are over-represented on organ transplant waiting lists. It is estimated that upwards of 50% of the people in Saskatchewan waiting for a kidney transplant are Indigenous, and approximately 30% will die because a kidney did not become available. However, while Métis and First Nations healthcare leaders identify organ donation and transplantation as an important health issue, they have limited resources to develop culturally safe-public education, -patient-centered care and -family supports. Over the past six months, our Think Tank members observed that Métis and First Nation people in Saskatchewan hold very diverse and complex understandings of organ donation and transplantation, and a range of factors, for example, where a patient lives, whether they have First Nations status or not, and the complexity of their health problems, directly impacts their decisions and experience as it relates to organ donor and transplantation. In our current provincial context, however, the voices of First Nations and Métis persons with lived experience (patients, caregivers and families) are muted. Our Network seeks to bring these voices, and the voices of our knowledge keepers, to the forefront through the expansion of our Think Tank and Network activities. Our work directly contributes to patient-centered research and knowledge translation, and addresses the lack of attention to this health issue in Saskatchewan and Canada generally.
This project supports five intersecting activities:
- The Saskatchewan First Nations and Métis Organ Donation and Transplantation Network Think Tank;
- A preliminary regional survey on First Nations and Métis perceptions of organ donation and transplantation, including the experience of patients, caregivers and families;
- Filmed interviews (6 patients and 6 knowledge keepers) focused on Métis and First Nation perceptions of organ donation and transplantation;
- Completion of a series of six painting by a Saskatchewan Woodlands artist that capture visually and artistically the voices of patients and knowledge keepers;
- Advance the development of culturally safe public education and patient care for First Nations and Métis patients, caregivers and families, pre- and post-organ donation and transplantation.
Our Partners
- The Canadian Donation and Transplant Research Program (CDTRP)
- Métis Nation - Saskatchewan (MN-S)
- Northern Medical Services
- Saskatoon Métis Local 126
- Kidney Foundation of Canada Saskatchewan Branch
- Canadian Blood Services


